While preparing for some recent LP presentations, we took a close look at all of…
Health / Biology
I’m scheduling my fourth knee surgery. But Ange… how is that possible when you only have 2 knees? Many years of playing Ultimate Frisbee… As I’m heading into this surgery, it has occurred to me that personalized medicine cannot come soon enough. Below I’m going to share my own health story and struggles associated with […]
While preparing for some recent LP presentations, we took a close look at all of…
Clayton Christensen has written the book on disruption. He’s one of Silicon Valley’s most popular…
I’m scheduling my fourth knee surgery.
But Ange… how is that possible when you only have 2 knees?
Many years of playing Ultimate Frisbee…
As I’m heading into this surgery, it has occurred to me that personalized medicine cannot come soon enough. Below I’m going to share my own health story and struggles associated with navigating a health system where there’s too much onus on the patient and too little coordination within the medical community. I’m sure that every single one of you has a similar story, or has a close friend or family member with a similar story as well…
Summer 2009, Toronto:
While playing ultimate, I was poaching off a weaker player and positioned myself between the opposing team’s handler and his six-foot-something teammate who was deep in the end zone. Just as I anticipated, the handler hucked the disc deep and I leapt as high as I could to intercept it. I blocked it but not before hearing a “pop”… sadly, my cleat caught the turf as I took off and I ended up tearing my ACL, MCL and meniscus. Surgery followed two months later to repair the tears in my right knee.
Fall 2012, Mountain View:
Three years post-op, I noticed that a bump had grown just above my incision scar. Given that I had moved to the Bay Area, I couldn’t see my Toronto surgeon and had to consult a local doctor. On a side note, the process of finding the “right” doctor in the US is such a terrible experience as many can attest. Is Yelp really the best resource for finding a medical professional? And yes, I am aware of the handful of startups solving this pain point. By contrast, in the single-payer (government) system of Canada, I had no choice and was “assigned” an orthopedic surgeon when I arrived at emergency / urgent care.
After an MRI, it was inconclusive as to what the root cause of the bump was but this new doctor suspected that my previous surgeon didn’t “seal the tunnel” where my knee was scoped. As a result, the cells “overly” proliferated at that site and formed a complex ganglion cyst. The only way to remove the cyst was to operate, so in January 2013, I had surgery #2 on my right knee.
Thanksgiving 2014, Palo Alto:
Back to playing ultimate…while on offense, I cut to the open side of my handler. Unfortunately, the disc slipped out of his hand and flew to the break side. To correct for this error, I tried to quickly change directions but as my body went one way, my left knee couldn’t keep up. Pop. A bad twist led to a torn ACL, MCL, and meniscus.
Now on a new insurance plan, the doctor in Mountain View who removed the right cyst was not “in-network” so I had to find a new orthopedic surgeon – cue Yelp again! I had surgery #3 in January 2015. This time, not only did I have a choice of doctor, but I also had a choice of procedure and graft (auto vs. allo). I couldn’t believe this decision was placed in my hands, and I couldn’t believe how indifferent the doctor was about which procedure was best. Was I really supposed to make this major medical decision with my limited experience and minimal information, when he had repaired 1000s of ACLs before mine? I informed him of the minor complication during my first surgery (which resulted in surgery #2) in hopes that it would narrow down my options. However, he believed that to be an independent event, and so I opted for the same treatment as my right knee because, cyst or no cyst, I knew that the repair was successful.
January 2017, Palo Alto:
Two years post-op, a cyst emerged just below my left knee – exactly in the same place as the right side. This can’t be a coincidence. I went back to my surgeon in Palo Alto and this time, I finally got an answer for the root cause: my body is incapable of breaking down the bioscrew originally anchoring my reconstructed ACL. A bioscrew is designed to degrade and be resorbed by the body after two years when the ACL is stable enough on its own.
In my case, however, my body recognized this bioscrew as a foreign object and in its defense, encapsulated it with tissue, leading to the formation of a cyst. “Why didn’t you tell me you were allergic to bioscrews”? my doctor asked.
Trying to keep my composure, I reminded him that I did mention that I had a cyst removed from my right knee but we didn’t know the root cause.
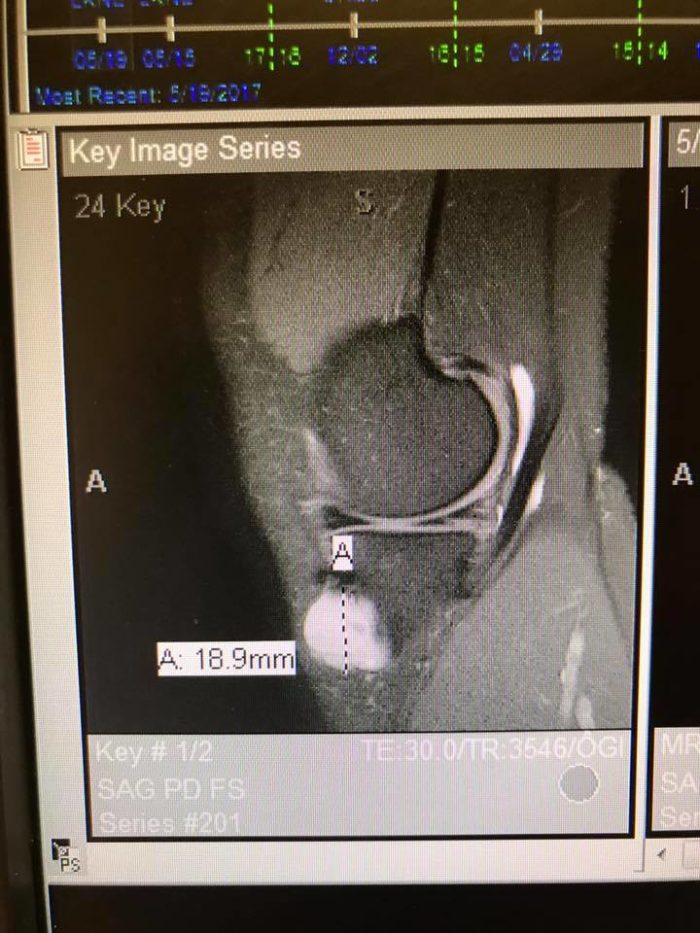
MRI of the ~2cm cyst in my left knee
Could I have avoided this 4th surgery? I’d like to think so. Not to place blame, but medical records could have been looked up and shared, especially in the instance where the patient (I) was unsure of all the details of the operations that she’s had. And even if I claimed to be 100% certain, should a doctor really take my word for it?
I asked my doctor if I’m an outlier. “This is not rare, but uncommon”, he answered. Ugh. If it’s not so uncommon, couldn’t I have been tested for bio-incompatibility somehow? What about future patients? At what point is the probability game not worth playing?
I recognize that the delivery of personalized medicine is not going to happen overnight. Beyond the technology, there is a coordination problem. This reminds me of the evolution of autonomous vehicles: there is no doubt that cars will be self-driving in the very near future, but adoption/policy is another story. Is our infrastructure built for this? Who will own the coordination network? Who will be responsible for mistakes?
Nonetheless, while we won’t ignore the effects of personalized medicine on our antiquated and regulated healthcare system, we will, for now, leave it to regulatory and policy makers, and focus on the technologies and innovations that will enable it altogether. Specifically, I’m excited by the potential of: 1) making it easier and cheaper to capture relevant data (i.e. cost of genomic sequencing is dropping); and 2) allowing for easier storage and access of this data (i.e. normalization and interoperability). Ultimately, these two data objectives will lend to the development of personalized treatment options, and hopefully with them, smart recommendations.
For those of you who have followed our blog over the years, you know that we have spent significant time on digital health (an oldie but goodie blog series here and an update from last summer here).
Now, we are also looking for companies that leverage strong network effects in bio/life sciences and genomics. In fact, we recently made our first two investments in this new category – both with the potential to contribute to personalized medicine: we announced our participation in Gencove two weeks ago and look forward to sharing more details on the other startup soon.
With that said, if you are working on democratizing medical knowledge, solving interoperability, and/or building unique bio banks / data sets, I’d love to talk to you.
P.S. I’m also happy to chat about Ultimate Frisbee or knees anytime 🙂
Portfolio
It’s been an eventful quarter (when has it not?), and somehow we’ve already crossed the halfway mark of 2025. We wanted to take a moment to highlight just a few of the wins, milestones, and momentum we’ve seen this past quarter. As always, there’s a whole lot happening behind the scenes that can’t be shared […]
The V1 family kicked off the new year with fresh energy and no shortage of…
At the end of Q1, we anticipated that a tech sector slowdown is ideal for…